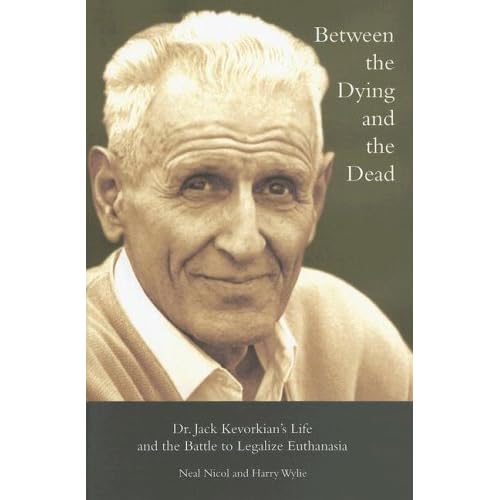
Dr. Jacob Kevorkian died this week. In case you don't know who he is
(where have you been living??? under a rock???) Wikipedia does a decent job of summarizing his life and his work here. Or you could read this book:He actually died in a hospital not far from where I live. I had no idea he was from Michigan. He was born in Pontiac, Michigan, about an hour north of me. He practiced medicine here (as a pathologist, not a general practitioner), did his research in transplants and transfusions here, and advocated much of his end of life beliefs in Michigan.
Whether or not you agree with his politics and convictions, you have to admit the guy had moxy and brought serious attention to a very valid issue in medicine today.
Now, be forewarned, this is not a commentary on my opinions about physician-assisted suicide. So please don't try to glean my thoughts on the matter from what I write here. If you want to know, please ask me directly, don't assume.
This is, however, a thought process on end of life issues that I am currently going through.
I am going to be a doctor one day, it is coming faster than even I realize, and the final days of a patient's life is something I need to know how to handle.
I admit, I have not been in the room during a "final code" on a patient, I haven't had to tell a patient's family that the patient died, nor have I had to look a patient and their family in the eye and tell them this is the end. I dread those moments with all my heart. I have no desire to be the one who has to drop that bomb and explain why what we did/are doing is not enough. It breaks my heart to even think about it. However, it is part of what I am choosing to do with my life and I pray for all the grace and peace in the world when those moments come.
But what breaks my heart even more, is seeing patients in the hospital connected to every machine possible to keep each organ functioning as close to normal as they can. I have seen this all too often.... How can that be considered good quality of life? Yes, it is life, but how would you feel being strapped to a bed surrounded by beeping, clanging, whooshing, clanking machines 24 hours a day, unable to move, not able to relieve yourself, at least not of your own will?
In the hospital, we have meetings for the students, residents, and physicians that are to specifically address Morbidity and Mortality. Notice they are not solely for "mortality", they consider "morbidity" too--that is the state or quality of life. Unfortunately, it is often we find that mortality is the common outcome of a hospital stay. But I wonder, of those patients that we keep alive with their colostomy bags, g-tubes, ventilators, and IV medications, fluids, food, how many are truly happy to be living that way? Yes, life is what we all want, but do we always inform our patients of what "choosing life" will actually mean for them in the long run? And what of their families? Are we even considering what we put their families through, especially now with insurance companies breathing down everyone's neck?
How many physicians take the time to sit down with each and every patient who is broaching a morbidity and mortality issue to discuss the possible outcomes and what they choose for their long term care? Sadly, I think it is very few. I have yet to see any physician do this.
Keith Olbermann has been very vocal about his thoughts on these issues. There was a great interview with him today on NPR regarding his outspokenness on this issue, specifically regarding the death of his father last year. I was really impacted by this today. He and his father had an extended period of time to discuss their choices for the end of his life. They were very fortunate in this, though they had recently dealt with the hospitalization and death of his mother so they were somewhat prepared for what might incur.
As I don't have any patients yet, I haven't spoken with any regarding this yet. I was afforded the chance to talk with my own family about it, very recently. In September, my dad was hospitalized for a number of days and my mom and I had some good discussions regarding his care and what she thought he would want. We were very fortunate that he came out alright with only a few life-long complications resulting. And then, a couple months later, my aunt was hospitalized and my dad, being the eldest and closest to her, had to make some tough decisions. He and I were able to have some very serious and poignant discussions about what was the right thing to do in these circumstances and what he thought would be best for his own long-term care.
For all those health professionals out there reading this, please consider having these discussions with your patients. Even if they're 85 and in great health, they are more likely than a 16 year old boy to get into a serious car accident, and then what do you do?
And for everyone else, I encourage you to bring up these conversations with your loved ones. It is unfortunate when we have to spend hundreds of thousands of dollars to keep trying to save someone who wouldn't have wanted the care anyway, but no one was there to tell us that.
Again, this is not meant to be a diatribe about end of life issues, but rather a discussion. I hope it brings thoughts and discussions to all who read it.
*Note: I am writing this and listening to Rosie Thomas. Her music inspires deep thoughts in me and I would recommend her for any thought provoking situation or rainy day or long walk.





















 Evenly layer your now juicy and well sugared rhubarb in the bottom of your pan
Evenly layer your now juicy and well sugared rhubarb in the bottom of your pan










 5. Grate up your ginger. doesn't that look delicious? still, not for eating just yet....
5. Grate up your ginger. doesn't that look delicious? still, not for eating just yet....